While traditional traumatic brain injury treatments have plateaued around rehabilitation and symptom management, researchers are discovering that psilocybin, the active compound in “magic mushrooms” may fundamentally rewire damaged neural circuits in ways previously thought impossible.
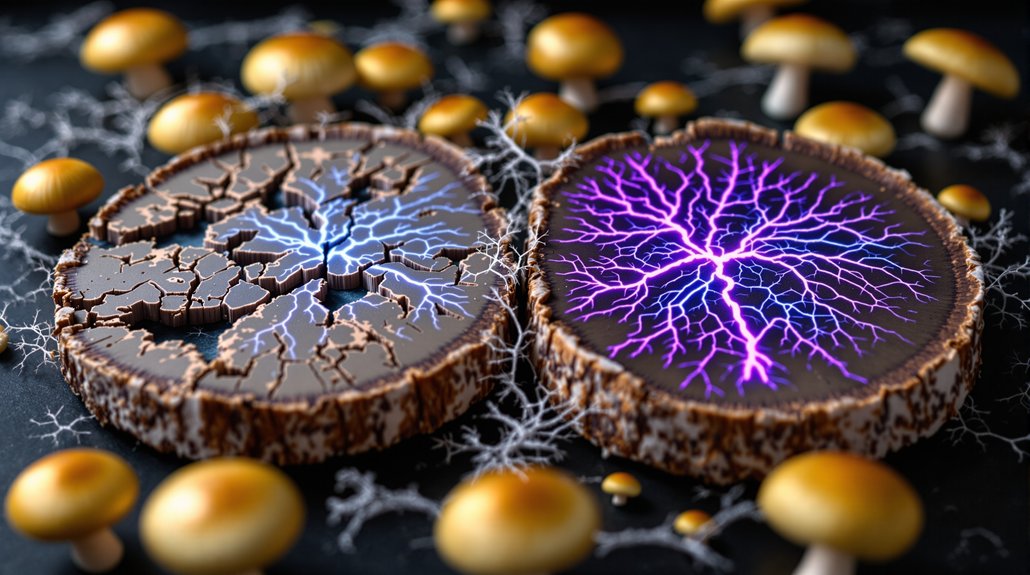
The science behind this potential breakthrough centers on neuroplasticity, the brain’s ability to form new connections and pathways. Psilocybin enhances neuritogenesis and synaptic plasticity in both animal models and human cortical tissues, essentially giving damaged brains fresh wiring instructions. Clinical imaging reveals something remarkable: the compound dissolves rigid connectivity patterns that typically trap TBI patients in cycles of cognitive and emotional dysfunction.
Psilocybin essentially provides damaged brains with fresh wiring instructions, dissolving rigid connectivity patterns that trap TBI patients in dysfunction cycles.
Perhaps most intriguing is psilocybin’s effect on the default mode network, the brain’s “screensaver” that becomes hyperactive in depression and anxiety. TBI patients often struggle with these psychiatric symptoms, which can derail recovery efforts. Psilocybin decreases connectivity between the DMN and anterior hippocampus for weeks after treatment, potentially breaking destructive thought patterns that conventional medications merely suppress.
The compound works through multiple biological pathways simultaneously. It activates 5-HT1A and 5-HT2A serotonin receptors while triggering TrkB neurotrophic signaling, which drives synaptic growth and recovery. Notably, researchers have identified that sigma-1 receptors also play a crucial role in psilocybin’s therapeutic mechanisms. This dual approach distinguishes psilocybin from other psychedelics, it’s not just altering perception but actively promoting neural repair.
Inflammation represents another battlefield where psilocybin shows promise. TBI triggers cascading inflammatory responses that often cause more damage than the initial injury itself. Multiple preclinical studies demonstrate psilocybin’s ability to reduce neuroinflammation by modulating microglial activity, the brain’s immune response system. Unlike MDMA which can cause neurological damage with repeated use, psilocybin appears to have neuroprotective qualities in controlled therapeutic settings. Direct comparisons with conventional anti-inflammatory drugs indicate similar or superior efficacy in certain animal models, without the side effect profiles that plague traditional medications.
Early human trials paint an encouraging picture. Phase 1 studies report cognitive enhancement following psilocybin administration, including improved attention and emotional processing. Veterans participating in retreat-based programs show normalized EEG connectivity patterns in emotional networks alongside improved mental health outcomes. These aren’t placebo effects; brain imaging confirms persistent structural changes weeks after treatment.
The research landscape remains nascent, with systematic clinical trials for TBI applications still needed. However, psilocybin’s robust performance in treating depression, PTSD, and addiction, conditions frequently complicating TBI recovery, suggest broader therapeutic potential. The compound appears to address not just symptoms but underlying neurobiological dysfunction. Studies indicate that psilocybin increases BDNF expression, which promotes neuroplasticity crucial for brain repair mechanisms.
This emerging science challenges fundamental assumptions about brain injury treatment. Rather than managing decline, psilocybin may offer genuine neural regeneration. For millions living with TBI consequences, that possibility represents hope where conventional medicine has offered primarily acceptance.